It seems ridiculous to ask anyone with a fever to wait in a holding pen full of people who are potentially infected with the Ebola virus for up to 24 hours before receiving a diagnosis. Yet right now, people in West Africa with anything from Lassa fever to Malaria are arriving at Ebola treatment centers to find out if they have the dreaded disease. And since they’ve had to wait a full day for results from a laboratory several miles away, they may have been exposed to Ebola unnecessarily.
Many people assume this absurd situation is due to poverty and the lack of infrastructure in West Africa, yet we tolerate similar situations almost everywhere in the world—including in the United States—every day.
Humans are terrible at timing when it comes to finding out how to effectively treat health problems. And we’re even worse at recognizing our bodies’ subtle cues that something might be wrong in the days, weeks, or even years leading up to a health crisis. Much of this stems from the fact that we normally wait for a problem to occur, and then we make an appointment to see a physician. This ancient paradigm is further complicated by the fact that physicians typically “outsource” diagnoses to analytical laboratories that put your samples in a testing queue. This cycle can take so long that, in many cases, treatment decisions have to be made based on the mere hope they will be effective. For example, doctors often prescribe antibiotics without knowing the underlying causes of infections. If they guess wrong, not only do they fail to cure their patients, they may be contributing to the worldwide crisis of antibiotic resistance.
When I began working in the field of clinical diagnostics back in 2001, the most forward-thinking companies planned to bring molecular tests (DNA or RNA) to the clinic. Many of the available technologies were capable of revolutionizing patient care by giving caregivers and patients the equivalent result of an automobile mechanic’s engine scanner. The Defense Advanced Research Projects Agency (DARPA) and other entities were eager to see these new technologies hit the commercial market, and they invested enormous amounts of money to make it happen. Yet in 2014, we still do not have a molecular test in the U.S. that’s cleared for use in clinics—or at home. They remain relegated to clinical laboratories scattered throughout the country.
It’s important to note that these tests were first developed in 1983, so we have waited more than three decades for them to show up at the bedside. Why have waited so long for such an effective technology to help us in diagnosis? I can tell you that almost all of the delay lies in the fact that we have created a very powerful lab diagnostic services industry (a global market expected to grow to $70B in 2017) which would like nothing better than to keep right on collecting reimbursements. Patients, however, must wait anywhere from 4 to 72 hours for results that can dictate the difference between one treatment decision or another—and even life or death.
All of this comes at a time when the ratio of patients to doctors is increasing. As a population, we are experiencing a shortage of care that is leading to unnecessary suffering and death. We only need to look at the recent scandal within the U.S. Department of Veteran’s Affairs to see the impact of an incorrect patient-to-caregiver ratio coupled with incompetent scheduling and prioritization. What if veterans could diagnose problems at home and upload results to the VA? The agency could then prioritize their visits based on those results, rather than some other non-medical criteria.
When the $2.25M Nokia Sensing XCHALLENGE was created, it sought to disrupt the status quo of limited access to health sensing, diagnostics, and delayed treatment. The technologies that were entered in the two competitions are capable of performing molecular tests, immunological tests, and monitoring a variety of vital signs. Nearly all have had some level of testing on real clinical samples, and have demonstrated the ability to transform healthcare. One product in the competition is capable of measuring pulmonary blood pressure (something that typically requires a costly catheterization in an advanced clinic or hospital) using an implant and hand-held reader. It allows cardiac patients to self-test at home and transmit their data directly to their healthcare providers on a daily (or more frequent) basis. The applications for this and related technologies go beyond providing a warning of an impending cardiac failure, they can also be used to fine-tune drug treatment regimens or trigger other lifestyle changes so a patient can avoid serious health outcomes.
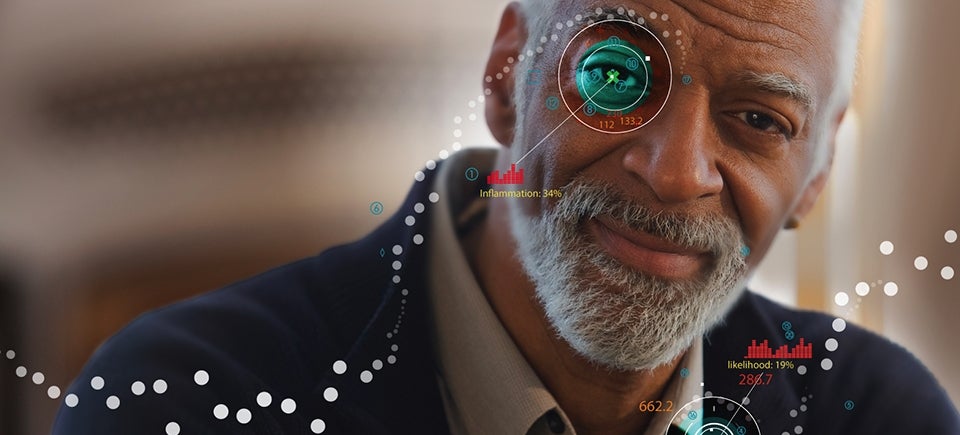
Making diagnostic products ubiquitous and operating on a continuous basis will not only serve to warn of pending health disasters, it will allow us to fine-tune treatment regimens and lead to the “N of 1” environment, in which a single patient is the subject of a clinical trial. Having the opportunity to fine-tune individual health pictures and optimize treatments will help minimize hospital visits and relieve the burden on an already-overwhelmed healthcare system. It will also incorporate the technologies and approaches pioneered by thousands of innovators involved in the “quantified self” movement.
What’s been shown repeatedly in other XPRIZE competitions is that success is not reserved only for the Grand Prize winners. InSilixa, a first round competitor and Distinguished Award winner in the Nokia Sensing XCHALLENGE, recently received private funding to produce a revolutionary, multi-target analysis that will enable hundreds (even thousands) of tests to be conducted on a patient sample via a proprietary array of sensors created using technology designed for printing integrated microchip circuits. This platform has already generated an impressive amount of clinical data and should be very effective in addressing problems ranging from multi-drug resistance, cancer, and even inherited disease. The potential for this technology to transform diagnosis at the point of care, or even at home, is immense—and will exponentially change the way we live.
Additionally, the winners of the two Nokia Sensing XCHALLENGE competitions have brought transformational technologies to the brink of becoming commercial products. The Grand Prize winner of the most-recent competition, Team DMI, developed the Reusable Handheld Electrolyte and Lab Technology for Humans (“rHEALTH”) system, a compact portable device that can run hundreds of clinical lab tests on a single drop of blood with gold standard accuracy, telling the user within minutes if they have a cold, the flu or a more serious ailment such as pneumonia — or even Ebola — that requires more urgent medical care. DMI’s unique ability to perform complete blood counts, as well as dozens of simultaneous assays using nanostrips, has literally brought a room full of lab equipment to the palm of your hand. But DMI didn’t stop there. They also created a continuous physiological monitoring system that, when paired with their sample-based analytical system, provides a highly integrated health picture that no other company has been able to provide. All of this is, of course, compatible with smartphone technologies that enable both doctors and patients to view results instantaneously, yet testing can be performed at home.
This competition has brought a wealth of technologies to the forefront that are not only capable of changing how patients receive care, but have the potential to transform how medications are monitored. The Nokia Sensing XCHALLENGE and its partner competition, the Qualcomm Tricorder XPRIZE, have coincided with an explosion of new technologies that are poised to re-shape our entire medical experience. With the emergence of Apple’s Health Kit and the dozens of wearable health monitors on the market that have the potential to interface with the major electronic health records companies, the wheels have been set in motion—and the exponential change we are about experience will be analogous to the changes we’ve seen in our society since the advent of the Internet.